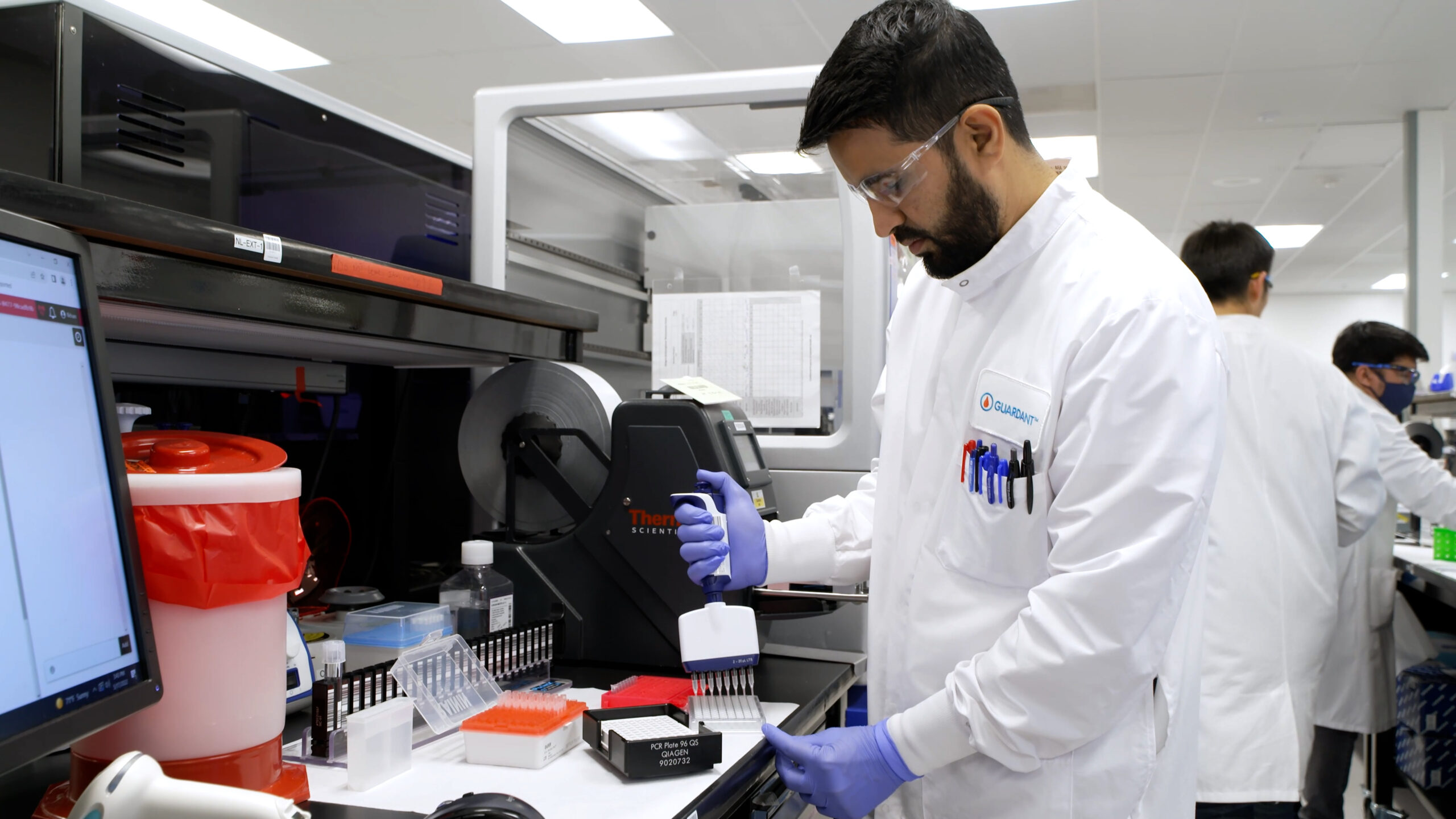
Publication of this article is supported by Guardant Health.
We all know, far too well, the toll that colorectal cancer (CRC) takes on the individuals and families it impacts. And in recognizing that each year, more than 150,000 new cases are reported – and nearly 53,000 lives are still lost[i] – we also know that our fight against the disease is far from over.
Recently our Sr. Director of Mission & Partnerships, Erin Peterson, sat down with Guardant Health’s Chief Medical Officer, Dr. Craig Eagle, to hear why he believes that hope – and positive change for colorectal cancer – may be on the horizon.
Erin Peterson: Thanks for joining me, Dr. Eagle. Before we begin, would you mind telling me a little bit about yourself?

Dr. Craig Eagle, Chief Medical Officer, Guardant Health
Dr. Craig Eagle: Thanks for having me, Erin, and sure. I currently serve as the Chief Medical Officer of Guardant Health, a precision oncology company that makes blood tests that not only help identify the presence and recurrence of cancer in patients, but that help inform and guide treatment decisions throughout a patient’s cancer journey. I’m a physician by training and have spent more than 20 years working in the oncology space, committed to trying to change the way we think about, and treat, cancer through the advent of innovation and technology.
EP: Thanks, Dr. Eagle. At the Colon Cancer Coalition, a big part of our mission centers around educating the public about the importance of colorectal cancer screening and helping to reduce barriers so that more people complete their screening.
Dr. Eagle: This is not only a noble mission, but a critical one, given that nearly 49 million Americans who should be screened are still walking around without having done so[ii] and because more than 75% of those who ultimately die from colorectal cancer were not up-to-date with their screening.[iii] For that reason, it’s actually become a part of our mission too.
EP: How so?
Dr. Eagle: At Guardant, we’ve always believed that if we truly want to help conquer cancer, we need to vastly improve the cancer screening landscape. So for the last four years, we’ve been working on creating and validating the effectiveness of a new screening option specifically for colorectal cancer: a convenient blood test that can be integrated into routine care with a simple blood draw and detect even the earliest signs of cancer.[iv]

Erin Peterson, Sr. Dir., Mission & Partnerships, Colon Cancer Coalition
EP: That’s amazing! We’ve been following the science around blood-based screening technology and are excited about all of the innovation emerging in this space.
Can you tell me more about your test? And what was the reason for starting with a screening test for CRC?
Dr. Eagle: We all know that survival outcomes are dramatically improved for colorectal cancer when it’s found early, through on-time screening. Five-year survival rates for stage I and stage II, for instance, can be as high 91%, as compared to 16% for stage IV.i So we know that CRC screening works; people just need to actually do it. And statistics unfortunately demonstrate that’s just not happening.
With one out of three eligible patients not up-to-date with screening today,[v] we’re not realizing the full benefits that screening can offer. What we are realizing, however, is that there are significant barriers to traditional screening methods keeping patients away.[vi] At Guardant, we see the need for a new option that can reach those who would otherwise remain unscreened, and more importantly, we see real potential to impact CRC screening rates and health outcomes if we can do so.
EP: Why a blood test? What can a blood-test do that other screening methods might not be able to?
Dr. Eagle: We believe that a blood-based option for CRC could help address many of the barriers that have historically limited people’s ability and willingness to get screened.vi It requires no special preparation, dietary changes, sedation, or extra time away from family or work – and it can be completed conveniently, in minutes, in most primary care offices during any doctor visit.vi With a blood test, patients can essentially be reached wherever they are.
EP: How does a screening test like this even work?
Dr. Eagle: As cancerous tumors grow they release DNA into the bloodstream. Our technology looks for this tumor DNA, called circulating tumor DNA – or “ctDNA” – to identify signals that are associated with colorectal cancer. If these signals are present, our test indicates an abnormal result and flags the patient as needing follow-up with a colonoscopy to determine if colorectal cancer is present.[vii] [viii] [ix]
EP: Where are you in the process with your test? Is it available now?
 Dr. Eagle: Our test, known as Shield™, has been commercially available in the United States since May 2022, and the insights we’ve been gathering – and the feedback we’ve been getting since it launched – have been very positive. Earlier this year, we also submitted our application for FDA approval of the test. Our ECLIPSE trial, which was just published in the New England Journal of Medicine served as the basis for the clinical performance to support our submission, and it demonstrated 83% sensitivity* in detecting colorectal cancer, with 90% specificity in the detection of advanced neoplasia, in a diverse and representative sample of over 20,000 individuals – spanning different ethnicities, races, and geographies across the United States.iv [x] We are hopeful we will receive FDA approval sometime in 2024, which would then start to broaden access to Shield to more people. It’s also important to note that our blood-based screening footprint now extends even beyond the US; Shield is currently available in Japan and Canada – with plans to expand even further throughout the world over time.
Dr. Eagle: Our test, known as Shield™, has been commercially available in the United States since May 2022, and the insights we’ve been gathering – and the feedback we’ve been getting since it launched – have been very positive. Earlier this year, we also submitted our application for FDA approval of the test. Our ECLIPSE trial, which was just published in the New England Journal of Medicine served as the basis for the clinical performance to support our submission, and it demonstrated 83% sensitivity* in detecting colorectal cancer, with 90% specificity in the detection of advanced neoplasia, in a diverse and representative sample of over 20,000 individuals – spanning different ethnicities, races, and geographies across the United States.iv [x] We are hopeful we will receive FDA approval sometime in 2024, which would then start to broaden access to Shield to more people. It’s also important to note that our blood-based screening footprint now extends even beyond the US; Shield is currently available in Japan and Canada – with plans to expand even further throughout the world over time.
EP: Once Shield is approved and more widely available, how are people supposed to choose which screening method is right for them? As a physician by training, how would you advise patients?
Dr. Eagle: In some cases, risk factors and family history will dictate the answer to that question. Colonoscopies, for example, are recommended for any individuals who are high-risk for CRC – based on a personal or family history – or who are experiencing symptoms.
But for those patients who are average risk, asymptomatic, and screen-eligible, there are obviously a few options, and a few factors to consider.
The first thing to look for when choosing a test is if it works and does the job it’s designed to do effectively. But alongside this, it’s just as important to consider how willing, able, or likely a patient is to take the test. Reason being: it won’t matter how effective a test is if people won’t take it. So, as the saying goes, I am a strong believer that “the best test is the one that gets done.” [xi]
Since we launched Shield for average-risk patients in 2022, we have reached thousands of individuals and are seeing more than 90% of them completing it[xii] , far outpacing the current adherence rate of ~65% across all other available screening options[xiii] and further reinforcing the ease of a test like this and patients’ preference for it.[xiv]
At the end of the day, we are hopeful that giving people more options in the screening process will empower them to get screened in a way that fits best with their lifestyle, needs, and overall preferences. As long as more people get screened, we will have succeeded.
EP: Isn’t that the truth!
Dr. Eagle: We sure think it is. CRC may be the second-leading cause of cancer related deaths in the United States,[xv] but it doesn’t have to be. If we can change the screening experience for patients with Shield, we’re hopeful that we may also be able to change their outcomes.
Shield may just require a simple blood draw, but it has the potential to also be a revolutionary test – especially if it helps us close the screening gap, once and for all!
EP: Will you keep us up to date on your progress, or let us know where people can go to learn more?
Dr. Eagle: Absolutely. We will make sure the Colon Cancer Coalition and your broader network receive news and updates as soon as they’re available. And if anyone has questions or would like to learn more in the meantime, they can visit www.bloodbasedscreening.com.
One day, we hope that no one has to die from colorectal cancer. And at Guardant, we are dedicated to playing our part in getting us there.
Thank you, Erin, for your time and this opportunity to share news about our work.
More About Guardant Shield
* Sensitivity refers to a test’s ability to designate an individual with disease as positive. The higher the sensitivity of a test, the fewer “false negative” test results there will be, and the fewer cases of disease that will be missed. The “specificity” of a test refers to its ability to designate an individual who does not have a disease as negative; the higher the specificity, the less “false positive” results there will be.
Shield™ is a qualitative laboratory developed test intended to detect colorectal neoplasia by identifying genomic and epigenomic alterations in cell-free DNA in plasma from blood collected in Guardant blood collection tubes.
- The assay is intended to be complementary to and not a replacement for current recommended colorectal cancer screening methods
- Patients with an “abnormal signal detected” Shield result should be referred for colonoscopic evaluation
- A “normal signal detected” Shield result does not preclude the presence of colorectal neoplasia, and patients should continue participating in guideline-recommended screening programs
- Shield was developed, and its performance characteristics determined, by the Guardant Health Clinical Laboratory in Redwood City, CA, USA, which is certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA) as qualified to perform high complexity clinical testing. This test has not been cleared or approved by the US FDA
References
[i] National Cancer Institute. Cancer Stat Facts: Colorectal Cancer. Cancer.gov website. Accessed October 19, 2023. https://seer.cancer.gov/statfacts/html/colorect.html
[ii] Colorectal Cancer Facts & Figures. American Cancer Society. 2020-2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2020-2022.pdf
[iii] Doubeni CA, Fedewa SA, Levin TR, et al. Modifiable failures in the colorectal cancer screening process and their association with risk of death. Gastroenterology. 2019;156(1):63-74. doi:10.1053/j.gastro.2018.09.040
[iv] Guardant Health announces positive results from pivotal ECLIPSE study evaluating a blood test for the detection of colorectal cancer. December 15, 2022. Accessed October 19, 2023. https://investors.guardanthealth.com/press-releases/press-releases/2022/Guardant-Health-announces-positive-results-from-pivotal-ECLIPSE-study-evaluating-a-blood-test-for-the-detection-of-colorectal-cancer/default.aspx
[v] Morrow L, Greenwald B. Improving the rate of colorectal cancer screening with the “80% in every community” campaign. J Am Assoc Nurse Pract. 2020 Jul 29;33(11):1035-1041. doi: 10.1097/JXX.0000000000000465. PMID: 32740330.
[vi] Rich T, Raymond V, Lang K. Where are we today? Efforts to understand strategies and barriers to physician issuance of a recommendation for colorectal cancer screening: a systematic review. Gastroenterology. 2020;158(6 suppl 1):S-918. doi:10.1016/S0016-5085(20)32981-4
[vii] Chung D, Gray DM, Greenson J, et al. 913e Clinical validation of a cell-free DNA blood-based test for colorectal cancer screening in an average risk population. Gastroenterology. 2023;164(6):S. doi:10.1016/S0016-5085(23)04760-1
[viii] Westesson O, Axelrod H, Dean J, et al. Integrated genomic and epigenomic cell-free DNA (cfDNA) analysis for the detection of early-stage colorectal cancer. Cancer Res. 2020;80(suppl 16):2316. doi:10.1158/1538-7445.AM2020-2316
[ix] Dean J, He Y, Raymond V, et al. Plasma based cell-free circulating tumor DNA (ctDNA) assessment for non-invasive detection of colorectal cancer (CRC). Gastroenterology. 2020;158(6 suppl 1):S-369. doi:10.1016/S0016-5085(20)31616-4
[x] Data on file. Guardant Health, Inc.
[xi] Bibbins-Domingo K, Grossman DC, Curry SJ, et al; US Preventive Services Task Force. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315(23):2564-2575. doi:10.1001/jama.2016.5989
[xii] Raymond VR, Foster G, Hong Y, et al. Implementation of Blood-Based Colorectal Cancer Screening: Real-World Clinical Experience. Poster presented at: American College of Gastroenterology; October 20-25, 2023; Vancouver, CA.
[xiii] U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2030: Increase the Proportion of adults who get screened for colorectal cancer – C-07. Accessed November 6, 2023: https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-proportion-adults-who-get-screened-colorectal-cancer-c-07
[xiv] Adler A, Geiger S, Keil A, et al. Improving compliance to colorectal cancer screening using blood and stool based tests in patients refusing screening colonoscopy in Germany. BMC Gastroenterol. 2014;14:183. doi:10.1186/1471-230X-14-183
[xv] American Society of Clinical Oncology. Colorectal cancer: statistics. Cancer.net website. Updated January 2021. Accessed October 19, 2023. https://www.cancer.net/cancer-types/colorectal-cancer/statistics

How much does guardant blood test cost?
Good Question, the cost of the Shield test may vary depending on a patient’s insurance coverage and the healthcare practice or provider who orders the test. Once Shield is approved by the FDA, however, it will be the first FDA-approved blood-based colorectal cancer screening test that meets the requirements for Medicare reimbursement, and Guardant Health – the manufacturer of the test – will be working with other payers at that time to expand access to the test with as little out-of-pocket costs as possible. For individuals who wish to self-pay for the test until then, the cash price is currently $895.